Introduction
Pneumoparotid is a rare cause of parotid gland swelling, and caused by retrograde air reflux from the oral cavity, into the parotid gland via Stensenâs duct [1-7]. Most patients complained of painless swelling in the parotid region [1-7]. Herein, we report a case of pneumoparotid, incidentally diagnosed without symptoms on computed tomography (CT), for follow-up of parotid lymph node enlargement.
Case report
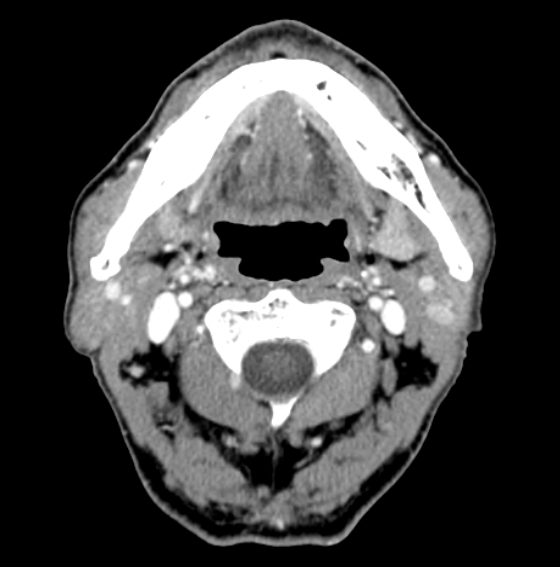
A 67-year-old man was referred to our department, with incidentally detected left parotid mass by radiologic examination. Physical examination revealed no palpable mass on the left parotid region. CT scans revealed a 1 cm sized enhancing nodular lesion in the left parotid gland (Fig. 1). We performed fine-needle aspiration cytology (FNAC) under ultrasonography (US), and the result was reactive lymphadenitis. One year later, CT was performed, to confirm the change in parotid lymph node size. The size of the lymph node was reduced, and there were no other abnormalities (Fig. 2).
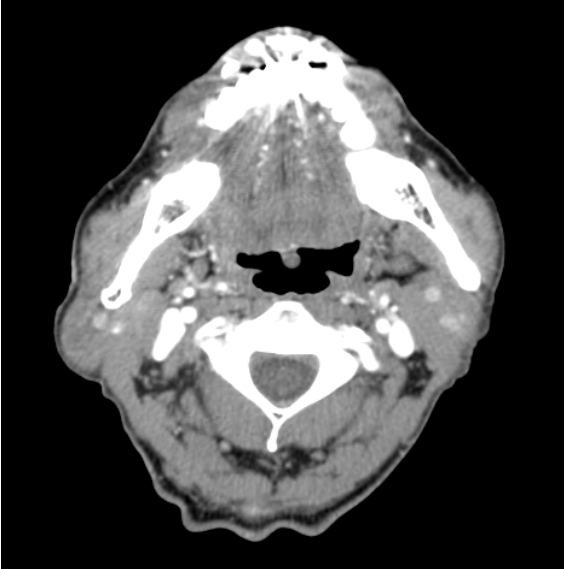
Periodic follow-up was performed, and the parotid lymph node disappeared on CT performed 3 years later. However, CT showed air in the parotid gland and Stensenâs duct, without subcutaneous emphysema or pneumomediastinum (Fig. 3). The patient presented no history of facial trauma, infection or surgical intervention. On physical examination, there was no swelling, tenderness, and subcutaneous emphysema on the left parotid gland. In addition, the patient had no symptoms and was observed without treatment. He remains free of symptoms at 1-year follow-up.
Discussion
Pneumoparotid is a rare condition, with air in the parotid gland [1-7]. It results from air reflux into the parotid gland, caused by high increase in intraoral pressure, which overcomes the parotid glandâs normal protective mechanism [1-7]. Therefore, pneumoparotid can occur due to an occupational hazard among wood wind performers and glassblowers, dental instrumentation, prolonged cough or nose blowing, complications of positive pressure ventilation or functional pulmonary exploration, playing wind instruments, in psychiatric disorder, or as an idiopathic finding [1,2,4,7]. We did not find the cause of pneumoparotid in this patient and thought it was idiopathic.
The presenting symptom of pneumoparotid is unilateral or bilateral parotid swelling, with or without tenderness [1-7]. In approximately 50% of patients with pneumoparotid, crepitus can be found in the parotid gland [1-5]. Frothy saliva or air bubbles from the Stensenâs duct orifice, can also be detected during compression of the parotid gland [1-5]. Extension of air may produce subcutaneous emphysema of the face and neck, pneumomediastinum, or pneumothorax [1,4,5]. In this case, he had no symptoms, but was incidentally diagnosed by radiologic examination.
The best diagnostic method for the pneumoparotid, is to confirm the air of the parotid gland, by radiologic examinations [1-7]. CT is standard examination, for diagnosis of pneumoparotid [1-4,6,7]. The puffed-cheek CT technique is very useful, for patients with clinically suspected pneumoparotid [2,3]. US, sialography and magnetic resonance imaging (MRI) also are effective, for diagnosis of pneumoparotid [1,4,6]. US can be used to exclude the presence of calculi and demonstrate air within the parotid gland [4,6]. Sialography can used to exclude calculi and may show air within the ducts or acini [2,6]. MRI helps to assess pneumoparotid complications [4]. MR-sialography showed duct dilatations in chronic parotitis [4]. In our case, we diagnosed pneumoparotid incidentally on CT, for follow-up of parotid lymph node enlargement.
Treatment of pneumoparotid can range from conservative, to surgical procedure [1,2,6,7]. Conservative management is targeted on avoidance of precipitating factors, such as high increase in intraoral pressure, and psychological or behavioral problems [1,2,6,7]. Most cases of pneumoparotid can be improved, with conservative and medical treatment [1,2,6,7]. Surgery is considered, only in patients with chronic or recurrent pneumoparotid, who fail conservative treatment [1,2,6,7]. Several surgical interventions have been described, including ligation of the Stensenâs duct orifice, transposition of parotid duct, and even parotidectomy [1,2,6,7]. This patient had no symptoms, and did not receive any treatment, and only observed periodically.
Pneumoparotid is a rare condition that causes air through the Stensenâs duct, to swelling of the parotid gland. Pneumoparotid should be considered part of differential diagnosis in patients with painless uni- or bilateral swelling of the parotid gland.