Introduction
Pilomatricoma was first introduced by Malherbe et al. in the late 1880s as a benign tumor with calcified epithelioma originating in the sebaceous glands.
1) In addition, using histological staining and electron microscopy, Forbis and Helwig discovered in 1961 that pilomatricoma occurs in hair matrix cells.
2)
The most frequently affected areas are the head and neck, followed by the upper extremities. Particularly in the head and neck, it is most frequent on the cheek, followed by the auricular area. The two most affected age groups are people in their 20s and 60s.
3)
Preoperative diagnostic methods for pilomatricoma include physical examinations and imaging. Ultrasound and computed tomography are helpful tools for diagnosing and evaluating pilomatricomas,
4,
5) According to Sung et.al., pilomatricoma have many variants such as anetodermic, aggressive, superficial, perforating, proliferating, ossifying, cystic, pigmented, acantholytic, and malignant types.
6) This diversity makes the accurate diagnosis of pilomatricoma difficult before surgery. Moreover, the pigmented type of pilomatricoma has rarely been reported, therefore it can be easily overlooked or misdiagnosed when evaluating the mass, even though imaging methods.
We report a case of pigmented pilomatricoma on the right ear triangular fossa that clinically mimicking hemangioma because of the high vascularity on the doppler ultrasound.
5)
Case
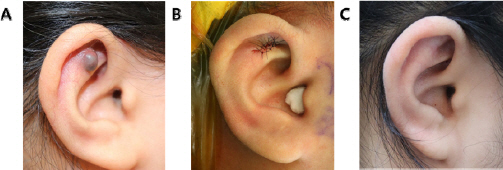
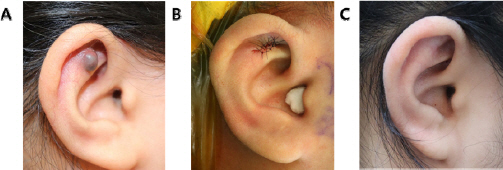
A 10-year-old girl visited our clinic because of a growing mass in the right ear triangular fossa. Upon physical examination a dark, bluish, round, protruding, and rubbery mass was observed (
Fig. 1A). Therefore, the mass was suspected to be of a primary vessel-derived mass. Ultrasonography was performed by a radiologist and showed a right ear mass of 0.7 x 0.5 x 0.8 cm that was identified as a hypervascular mass in the subcutaneous fat layer, which could be a benign soft tissue lesion or vascular tumor (
Fig. 2).
Fig.┬Ā1
(A) A 10-year-old female patient visited the plastic surgery clinic because of a mass on the right ear triangular fossa. The mass was cystic, rubbery, and movable, with a dark purple color. (B) Immediate postoperative state. (C) Good postoperative state 1 year after surgery.
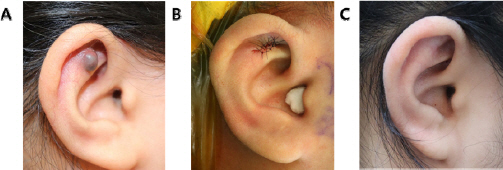
Fig.┬Ā2
About 0.7 x 0.5 x 0.8 cm sized hypervascular mass in subcutaneous fat layer of right ear, palpable area. (A) Ultrasonography without doppler signal (B) Doppler view.

Subsequently, the mass was totally excised without perichondrial invasion. The vascular component was not observed grossly. After the resection, a 2.0 cm x 1.5 cm defect was covered by a local flap, and surgery was completed with a compression dressing. The 1-year follow-up showed satisfactory results without recurrence or scarring (Figs.
1B,
1C).
In pathological examination, the proliferated basaloid cells and ghost cells show no nuclear atypia and black pigments in the cytoplasm. Central area of the tumor reveals many dilated vascular structure. Immunohistochemically, the tumor cells show positive for HMB45, Melan A and S100 (
Fig. 3). The microscopic features and immunohistochemical expressions confirm that this tumor is a pigmented pilomatricoma.
Fig.┬Ā3
Pathological features of the pigmented pilomatricoma. (A) The specimen shows areas of proliferated basaloid cells (white arrow) and ghost cells (black arrow), and central dilated vascular structures (arrow head). (B) High magnification of Fig. 4A (white squared area), both proliferated basaloid cells (white arrow) and ghost cells (black arrow) show abundant black pigments in cytoplasms. (C-E) Immunohistochemically, the melanocytic basaloid cells show positive expressions for HMB45 (C), Melan A (D) and S100 (E). Original magnification, A: x50, B: x200, C-E, x200

Consideration
Pilomatricoma is a benign tumor that originates from the epidermal hair matrix. Pilomatricoma occurs mainly in the head and neck, followed by the upper limbs.
4) It is known to occur mainly in children aged < 20 years and in women rather than men. Pilomatricoma has various phenotypes, such as anetodermic, aggressive, superficial, perforating, proliferating, ossifying, cystic, pigmented, acantholytic, and malignant.
6) Owing to this variety, pilomatricomas are often mistaken for other tumors.
7)
Preoperative imaging methods include ultrasonography, computerized tomography, and magnetic resonance imaging, with the most useful being ultrasonography, as it is noninvasive and provides relatively accurate results. However, the most crucial diagnosis aspect is the pathologic study, in which characteristic central eosinophilic and ghost cells are observed.
The ultrasonographic findings of pilomatricoma represents calcification in hypoechoic area, hypoechoic rim, posterior acoustic shadowing, and peritumoral hyperechogenicity. However, the hemangioma also presents as well defined, hypoechoic tumor on ultrasound. The most characteristic findings and also differentiating points from hemangioma of pilomatricoma are calcification and hypoechoic rim.
5)
Pigmented pilomatricoma, which has melanocytes or melanin pigments within the cytoplasm of proliferated basaloid cells without nuclear atypia, has rarely been documented. To demonstrate the presence of melanin, immunohistochemical stains were performed for HMB45, Melan A and S-100.
8) Rapid tumor growth can cause internal bleeding, which leads to hemosiderin pigmentation. Such pigmentation leads to the pigmented pilomatricoma mimicking as vascular-origin tumor or skin cancers with pigmentation.
9)
This study introduces a case of a mass thought to be a vascular origin on ultrasonography, which is known to be useful for diagnosis, but confirmed as pilomatricoma on histological examination. Pilomatricomas mainly show calcification and hypoechoic rim on ultrasound; however, in the present case, calcification and hypoechoic rim were absent and represent relatively high vascularity. In addition, because of the apparent dark and bluish color, hemangioma was suspected.
If it is mistaken for a hemangioma, the treatment methods may differ. The treatment of hemangiomas includes operative and nonoperative methods. Nonoperative treatment for hemangioma includes observation for spontaneous regression, topical corticosteroid, intralesional corticosteroid, topical timolol, and systemic pharmacotherapy.
10)
Performing treatment for hemangioma in the case of pilomatricoma can deteriorate the situation. Surgery may become more complicated, leading to an increased risk of complications, such as scarring, and increased risk of recurrence. Although rare, pilomatricoma can also potentially become malignant, which is aggressive and has a high rate of relapse.
11) Therefore, it is critical to consider the differential diagnosis of pilomatricoma even if it appears to be another kind of tumor and perform surgical excision and histological examination whenever possible.
In conclusion, when treating pigmented lesions especially in the head and neck area of children, pigmented pilomatricoma should be considered and precise preoperative evaluation should be performed.